Alzheimer’s disease (AD)
Alzheimer is named after Dr. Alois Alzheimer who noticed changes in the brain tissue of a woman who had died of an unusual mental illness. Her symptoms included memory loss, language problems, and unpredictable behavior.
Alzheimer's disease is the most common cause of dementia among older people. The prevalence of AD is strongly age-dependent - doubling every 5 years after the age of 60 years with around 1% of those aged 65-69 years affected rising to almost 20% in those aged 85 years or over.
Dementia is the loss of cognitive funcationing -thinking (processing of information), remembering (episodic memory), reasoning, language (aphasia), motor activities (apraxia), recognize or identify objects (agnosia) - to such an extent that it interferes with a person's daily life and activities.
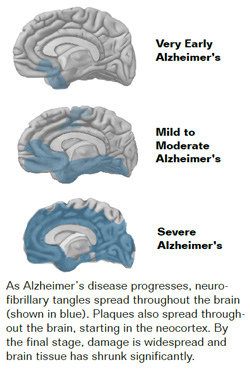
A definitive diagnosis of AD requires histopathological examination of brain tissue demonstrating excess accumulation of extracellular amyloid plaques and intracellular neurofi brillary tangles. In established AD, amyloid plaques are found widely distributed throughout the cortex with heaviest deposition in the cortical association areas.
Etiology
Clearly age is the biggest risk factor for AD. One of the great mysteries of AD is why it largely strikes older adults. Age-related changes in the brain may harm neurons and contribute to Alzheimer's damage. These changes seen in brains of older people are atrophy (loss of neurons in critical brain areas), inflammation, and production of unstable harmful molecules called free radicals.
Mutations in three genes are known to cause autosomal dominant AD with a high level of penetrance and usually with an early age at onset. Together these mutations account for only 1% of all cases of AD.
Mutations in the Presenilin-1 gene (PS-1) on chromosome 14 account for approximately 50% of all autosomal dominant familial AD and often have the youngest age at onset: typically between 35 and 50 years of age but may be as early as 30 years and may occasionally present after the age of 65 years. The other mutations are PS-2 and APP. Overall, a family history of AD in a first degree relative occurring at any age confers an approximately twofold increase in an individual's lifetime risk.
Recurrent head injury (as in boxers), down syndrome, late life depression are other risk factors for AD.
Most people with AD have late-onset Alzheimer's, which usually develops after age 60. Most experts believe that additional genes may influence the development of late-onset Alzheimer's in some way.
Symptoms and diagnosis
Obtaining a reliable history is key to the diagnosis. The most common complaint, often made by spouse or other family member is of problems with memory. The gradual development of forgetfulness is the major symptom. Patients become repetitive in questioning, forgetting that they asked the same question recently. There is progressive difficulty often with misplacing items (e.g. keys, glasses). Language problems develop, like naming difficulties (dysnomia) and may first bring the patient to a neurologist. Many of these symptoms may be seen during normal ageing. In AD the severity of the symptoms progress over time. These early symptoms reflect impairment of episodic memory. However, an isolated memory deficit is not sufficient for a clinical diagnosis of AD. Diagnostic criteria for AD require deficits in multiple cognitive domains of sufficient severity to impair activities of daily living.
Patients may have objective deficits of episodic memory without any other cognitive impairments and may have little problem continuing their activities of daily living. These patients are called as 'Amnestic Mild Cognitive Impairment' (MCI). About 10% of patients with MCI progress to AD every year. Which patients will progress to AD is difficult to predict. Generally, those patients with multiple cognitive deficits (amnestic + non-amnestic) are more likely to develop AD.
As the disease progresses cognition worsens. There is impairment of orientation and the patient may get confused or lost in familiar surroundings. Deterioration in an individual’s ability to drive and judgment may lead to accidents. There are impairments of planning, decision-making and working out complex sequences, and learning new tasks. The patients no longer read as much as they have before. With time, problems with speech and naming become increasingly marked, eventually leading to significant impairment of communication. In advanced stages the patient is dependent on all activities like eating, drinking, wearing clothes, walking. The patient gets wheelchair bound and later bed bound. Feeding tube and urinary catheter may be needed. Typical AD progresses slowly over 10 to 15 years.
Investigations and diagnosis
In clinical practice. There are no laboratory diagnostic tests for AD. The diagnosis is of exclusion. Research criteria based on combination of biomarkers and imaging are used for diagnosis in studies. It is important to exclude alternative causes of cognitive decline. It is essential to treat with antidepressants and see the response, especially in the early stage of disease if depressive features are prominent. All patients with dementia should undergo structural imaging (CT or MRI) as part of their diagnostic work-up. AD is associated with marked and disproportionate medial temporal lobe atrophy, which is best seen with MRI using a coronal T1-weighted volumetric sequence. PET and SPECT scans, show symmetrical temporo-parietal hypometabolism and hypoperfusion. It is important to note that structural and functional (PET) scans are normal in the early stages of disease.
EEG may be important to exclude seizure activity as a relatively uncommon cause of memory impairment and, if this is suspected, prolonged recordings may be required. In AD the EEG typically shows generalized slowing and loss of alpha rhythm, although in mild cases may appear normal.
Treatment
An approach which covers social support, advice on legal issues, benefit and support issues is essential. Treatment of depression must be considered as discussed earlier. Specific symptomatic pharmacological treatments for AD are the cholinesterase inhibitors and memantine, an NMDA antagonist.
The cholinesterase inhibitors, (AChEIs) are used for symptomatic treatment of AD. In the cerebral cortex of patients with AD there is reduced activity of the enzyme choline acetyltransferase, with subsequent reduction in cortical levels of the neurotransmitter acetylcholine (ACh). By inhibiting the breakdown of ACh, AChEIs enhance the levels of ACh in cerebral cortex. There are currently three AChEIs available for the treatment of mild to moderate AD: donepezil, galantamine and rivastigmine. The use of AChEIs in dementia is a debated subject since the response to treatment
may be limited in the majority. However, even small effects can significantly benefit quality of life for patients and care givers. Around 20% patients may have a dramatic response to AchEIs.
Memantine prevents glutamate-mediated neurotoxicity. It is a voltage-dependent N-methyl-d-aspartate (NMDA)-receptor antagonist. It has beneficial effects in slowing cognitive decline in mild to moderate AD.
Treatment is essentially symptomatic and AD is an irreversible, progressive brain disorder which gradually affects all cognitive aspects.
Supporting families and caregivers of AD
Caring for a person with Alzheimer’s disease can have high physical, emotional, and financial costs for the family. Becoming well-informed about the disease is one important long-term strategy. Developing good coping skills and a strong support network of family and friends are important ways that caregivers can help themselves handle the stresses of caring for a loved one with AD.
Preventing AD
A nutritious diet, physical activity, social engagement, and mentally stimu-lating activities can all help people stay healthy. Mediterranean diet is advised and thought to be protective for AD. Vascular and metabolic conditions such as heart disease, stroke, high blood pressure, diabetes, and obesity may have an adverse effect on cognition. Reducing risk factors for these diseases may help with AD progression and preventing additional cognitive loss.
Patient's Education
- Epilepsy
- Parkinson Disease
- Migraine
- Stroke
- Bell facial palsy
- Tension type headache
- Alzheimer dementia
- Vertigo
- Neurocysticercosis
- Cerebral venous sinus thrombosis
- Motor neuron disease
- Myasthenia gravis
- Carpal tunnel syndrome
- Wilson disease
- Meningitis
- Febrile Seizures
- Medication overuse headache
- Back pain
- Demyelination and Multiple Sclerosis
- Facial pain
- Neck Pain
- Trigeminal Neuralgia