Epilepsy is one of the most common disorders of the brain. One of every ten people will have at least one epileptic seizure during a normal lifespan, and a third of these will develop epilepsy. Epilepsy is, not a specific disease, or a single syndrome, but rather a broad category of symptom complexes arising from any number of disordered brain functions that themselves may be secondary to a variety of pathologic processes.
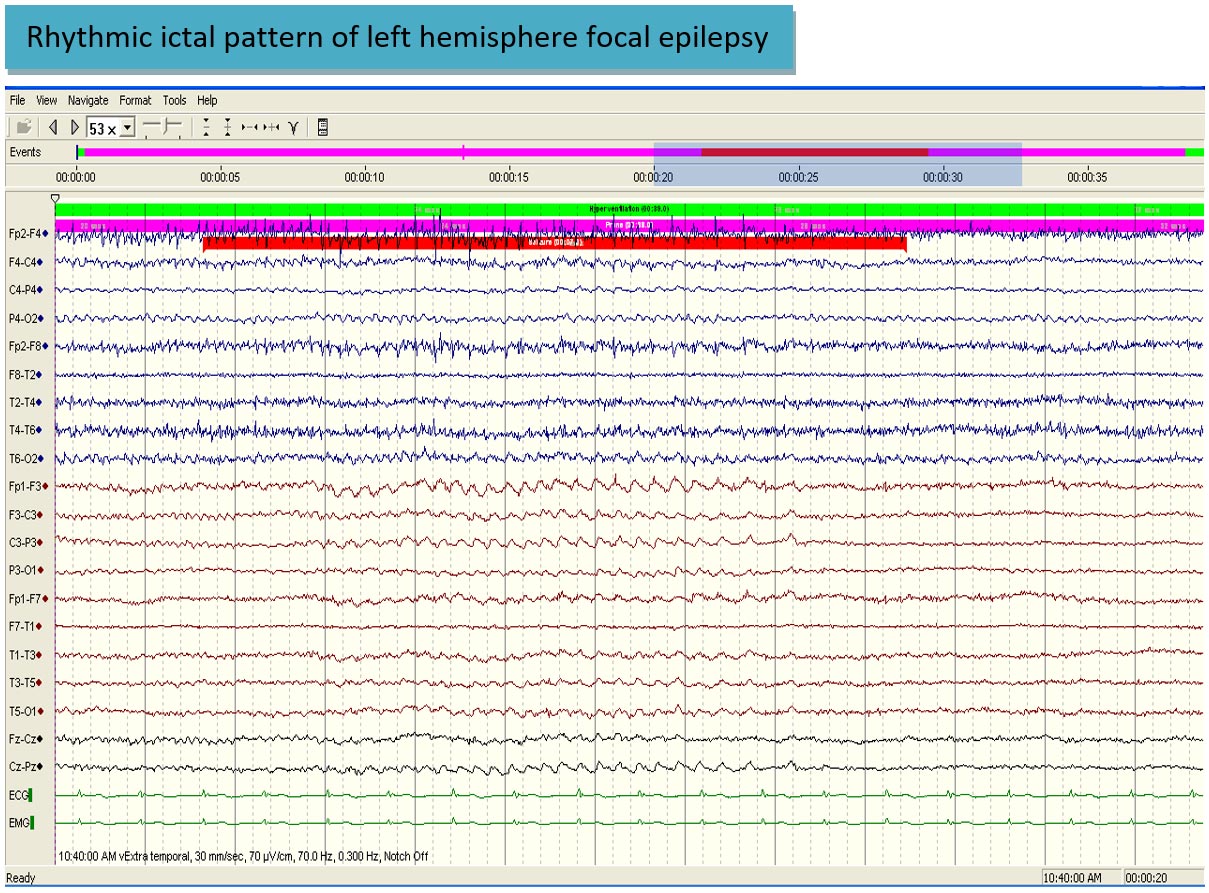
All patients with epilepsy have seizures but not everybody who has seizures has epilepsy. Epilepsies are a group of neurologic disorders characterized by recurrent unprovoked seizure. Thus epilepsy is not one disease and different people with a diagnosis of epilepsy can have totally different symptoms and treatment. A seizure is a manifestation of an electrical disturbance in the brain. An epileptic seizure is the manifestation of an abnormal, hypersynchronous discharge of a population of cortical neurons. This discharge may produce subjective symptoms or objective signs, in which case it is a clinical seizure, or it may be apparent only on an electroencephalogram (EEG), in which case it is an electrographic (or subclinical ) seizure.
International Classification of Epileptic Seizures
- Focal onset seizures
- Focal onset seizures with awareness preserved
- With motor signs
- Focal motor without march
- Focal motor with march (Jacksonian)
- Versive
- Postural
- Phonatory
- With somatosensory or special-sensory symptoms
- Somatosensory
- Visual
- Auditory
- Olfactory
- Gustatory
- Vertiginous
- With autonomic symptoms or signs
- With cognitive symptoms
- Dysphasia
- Dysmnesic
- Affective
- Illusions
- Structured hallucinations
- With motor signs
- Focal onset seizures with impaired awareness
- Focal seizures at onset, followed by impairment of awareness
- With focal features, no automatsm
- With automatisms
- With impairment of awareness at onset
- With impairment of awareness only
- With automatisms
- Focal seizures at onset, followed by impairment of awareness
- Focal seizures evolving to bilateral tonic clonic seizures
- Focal seizures evolving to bilateral tonic clonic seizures
- Focal seizures with impaired awareness evolving to bilateral tonic clonic seizures
- Focal seizures with awareness evolving to impaired awareness evolving to bilateral tonic clonic seizures
- Focal onset seizures with awareness preserved
- Generalized seizures
- Absence seizures (non-motor)
- Typical absence seizures
- Impairment of awareness only (non-motor)
- With mild clonic components
- With atonic components
- With tonic components
- With automatisms
- With autonomic components
- Atypical absence seizures
- Typical absence seizures
- Myoclonic seizures
- Clonic seizures
- Tonic seizures
- Tonic-clonic seizures
- Atonic seizures
- Absence seizures (non-motor)
- Unknown onset
- Motor
- Non motor
- Unclassified
Classification of Epilepsy syndromes
International Classification of Epilepsies and Epileptic Syndromes
- Focal epilepsies and syndromes
- Idiopathic with age-related onset
- Benign childhood epilepsy with centrotemporal spikes
- Childhood epilepsy with occipital paroxysms
- Symptomatic
- Chronic progressive epilepsia partialis continua of childhood
- Syndromes characterized by seizures with specific modes of precipitation
- Temporal lobe epilepsies
- Frontal lobe epilepsies
- Parietal lobe epilepsies
- Occipital lobe epilepsies
- Crytopgenic
- Idiopathic with age-related onset
- Generalized epilepsies and syndromes
- Idiopathic, with age-related onset (listed in order of age)
- Benign neonatal familial convulsions
- Benign neonatal convulsions
- Benign myoclonic epilepsy in infancy
- Childhood absence epilepsy (pyknolepsy)
- Juvenile absence epilepsy
- Juvenile myoclonic epilepsy (impulsive petit mal)
- Epilepsy with grand mal seizures on awakening
- Other generalized idiopathic epilepsies not defined above
- Epilepsies with seizures precipitated by specific modes of activation
- Idiopathic and/or symptomatic (listed in order of age)
- West syndrome (infantile spasms)
- Lennox-Gastaut syndrome
- Epilepsy with myoclonic-astatic seizures
- Epilepsy with myoclonic absences
- Symptomatic
- Nonspecific etiology
- Early myoclonic encephalopathy
- Early infantile epileptic encephalopathy with suppression burst
- Other symptomatic generalized epilepsies not defined above
- Specific etiology
- Epileptic seizures may complicate many disease states
- Nonspecific etiology
- Idiopathic, with age-related onset (listed in order of age)
- Epilepsies and syndromes undetermined as to whether they are focal or generalized
- With both generalized and focal seizures
- Neonatal seizures
- Severe myoclonic epilepsy in infancy
- Epilepsy with continuous spike waves during slow-wave sleep
- Acquired epileptic aphasia (Landau-Kleffner syndrome)
- Other undetermined epilepsies not defined above
- Without unequivocal generalized or focal features
- With both generalized and focal seizures
- Special syndromes
- Situation-related seizures
- Febrile convulsions
- Isolated, apparently unprovoked epileptic events
- Seizures related to other identifiable situations such as stress, hormonal changes, drugs, alcohol, or sleep deprivation
- Situation-related seizures
Classification of the Epilepsies
Common seizure types
Focal seizures
With awareness (previous terminology - Simple partial seizures)
These are defined as partial seizures in which consciousness is not impaired.
With impaired awareness (previous terminology-Complex partial seizures)
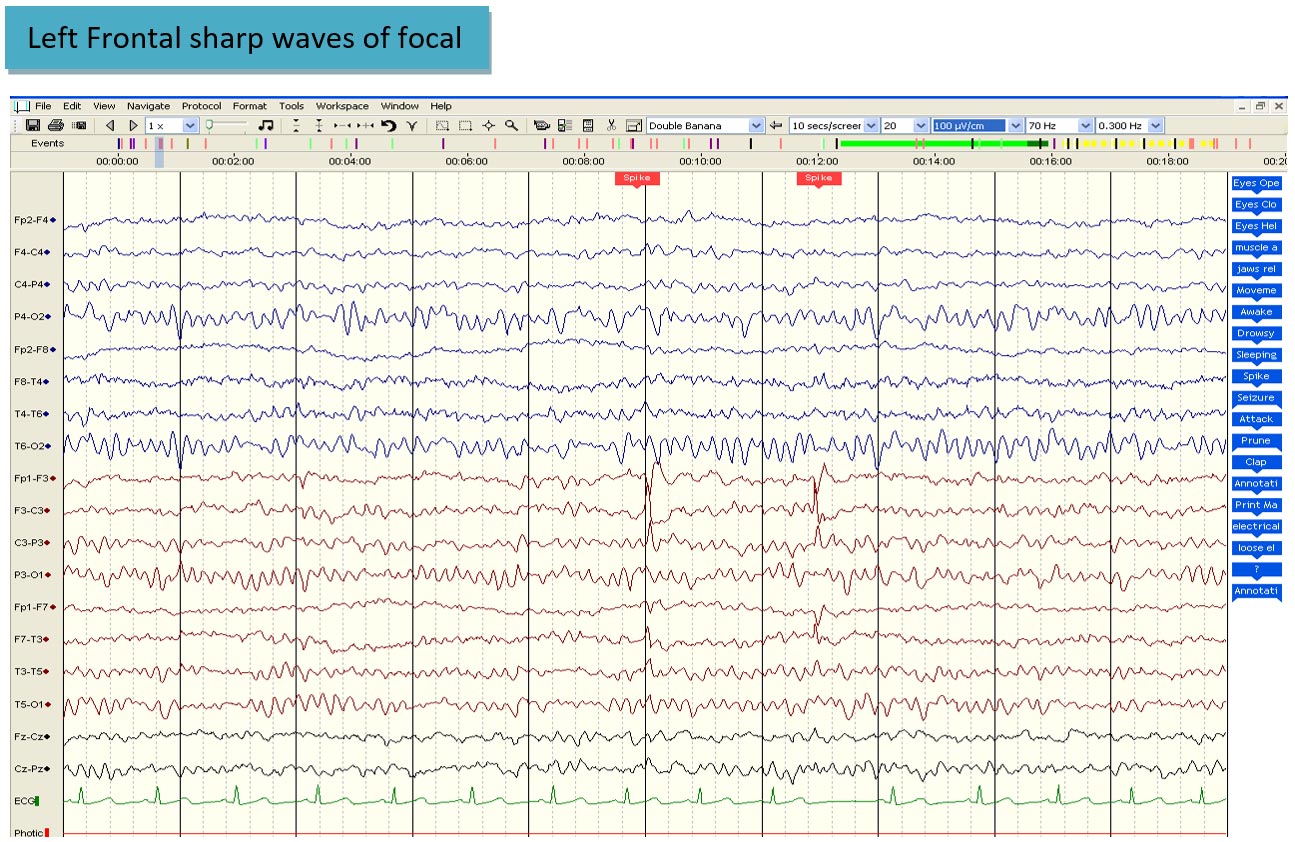
Complex partial seizures are those in which consciousness is impaired. Both simple and complex partial seizures imply focal cerebral disease and seizures can arise from any cortical region, the most common sites being the frontal and temporal lobes.
With awareness
Motor manifestations can include jerking, spasm or posturing, speech arrest, dysarthria, choking sensations, version of the head or eyes or, less commonly, rotation of the whole body can occur in epilepsy arising in many cortical areas. Visual phenomena such as flashing lights and colors occur if the calcarine cortex is affected. A rising epigastric sensation is the most common manifestation of a simple partial seizure arising in the mesial temporal lobe. Illusions of size (macropsia, micropsia), shape, weight, distance or sound are usually features of temporal or parieto-occipital epileptic foci. Dysmnestic symptoms (disturbance of memory) such as flashbacks, déjà vu, jamais vu, or distortions of memory are most common in mesial temporal lobe seizures although also occur in inferior frontal or lateral temporal lobe seizures. Hallucinations of taste, usually an unpleasant taste, are a frequent symptom of temporal lobe epilepsy. Visual hallucinations can vary greatly in sophistication from simple colours or flashing lights in epilepsy arising in calcerine cortex.
With impaired awareness
It is possible to identify three distinct components: the aura, the absence or a dialeptic phase (loss of consciousness) and the automatism in a complex partial seizure. These arise from the temporal lobe in about 60% of cases.
The aura is in effect a simple partial seizure. It is usually short-lived, lasting a few seconds. During the dialeptic phase the patient usually appears to be staring, is unresponsive to the environment and has no memory for the ensuing period. Automatisms are defined as involuntary motor actions that occur during or in the aftermath of epileptic seizures, in a state of impaired awareness. The most common automatisms are oro-alimentary automatisms in which orofacial movements occur such as chewing, lip smacking, swallowing or drooling, gestural automatisms include fiddling movements with the hands, tapping, patting or rubbing, ordering and tidying movements. The patient is usually totally amnesic for the events of the automatism.
Generalized seizures
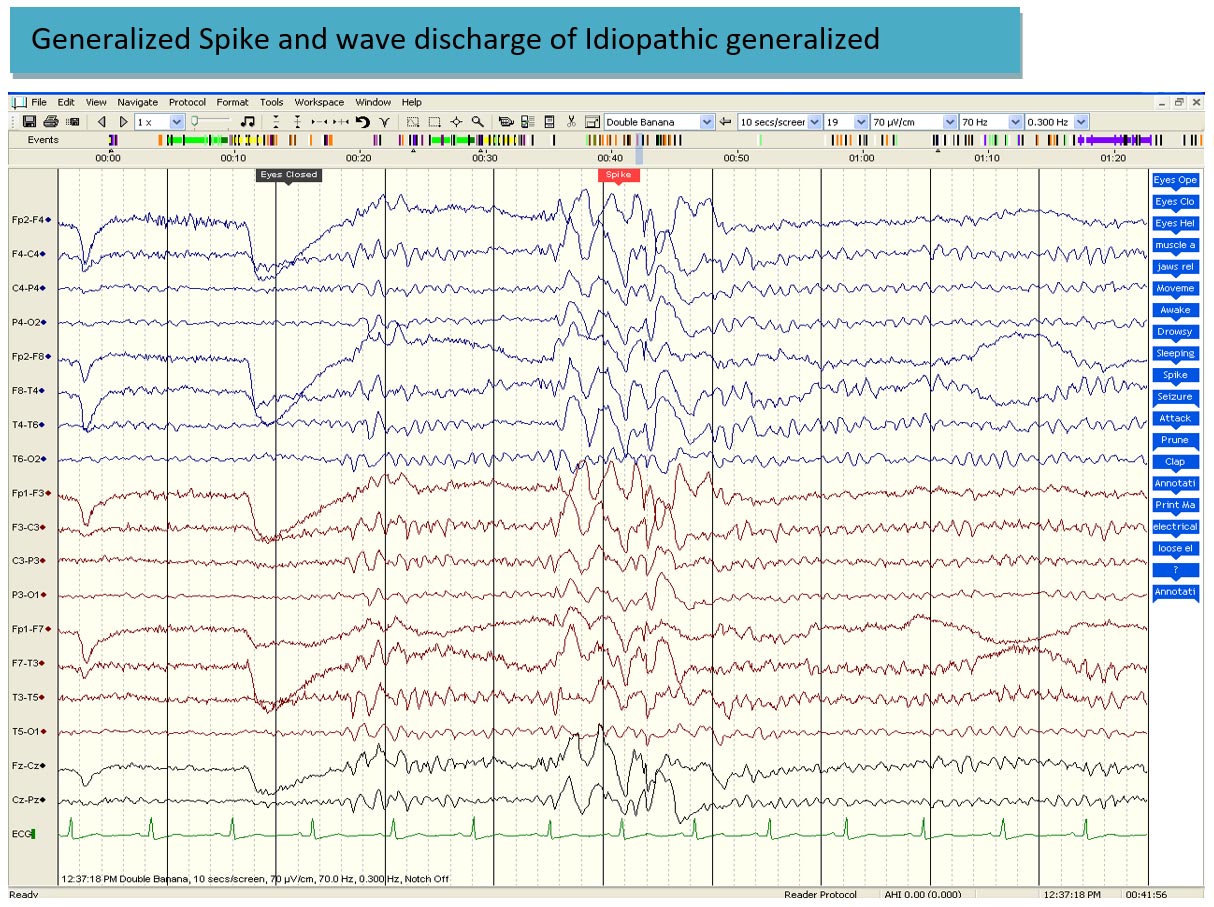
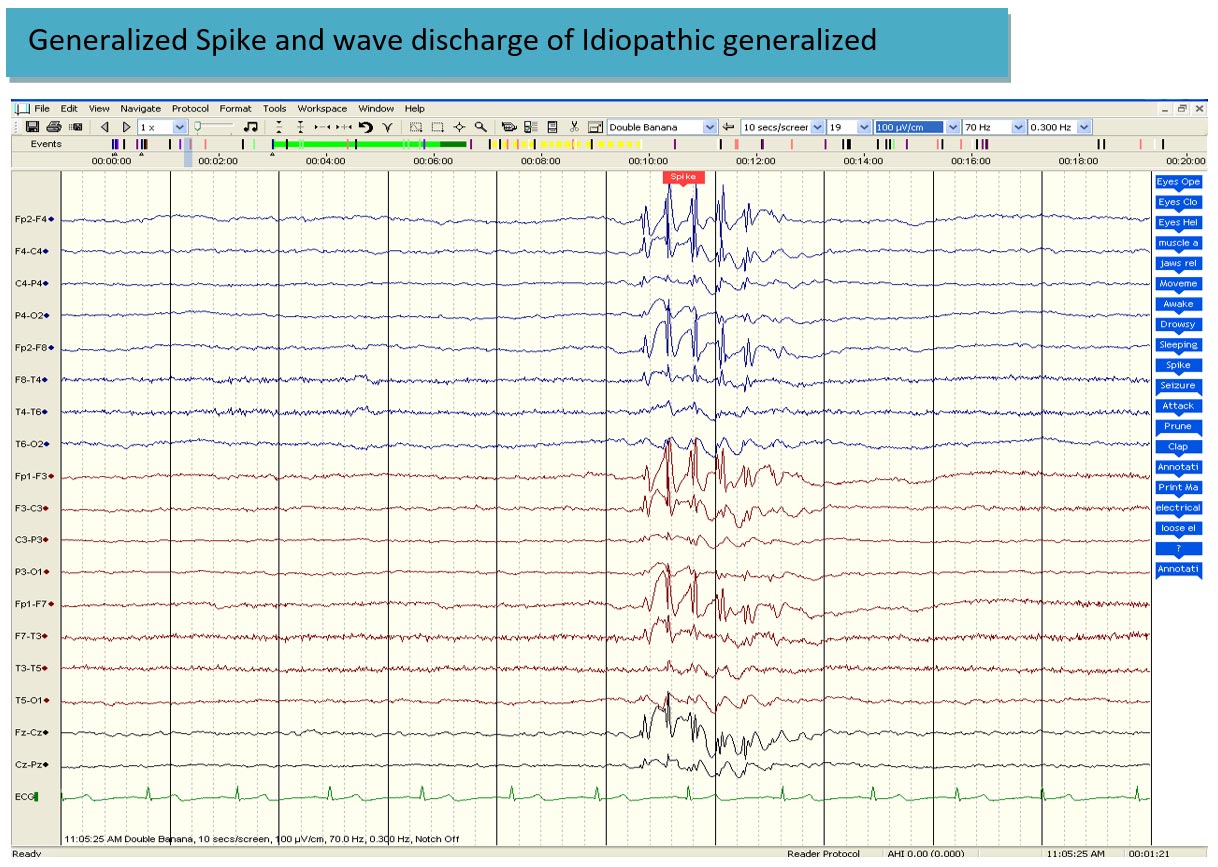
In generalized seizures consciousness is impaired from the onset of the attack, motor changes are bilateral and more or less symmetric, and the EEG patterns are bilateral and grossly synchronous and symmetrical over both hemispheres.
Typical absence seizure (petit mal seizure)
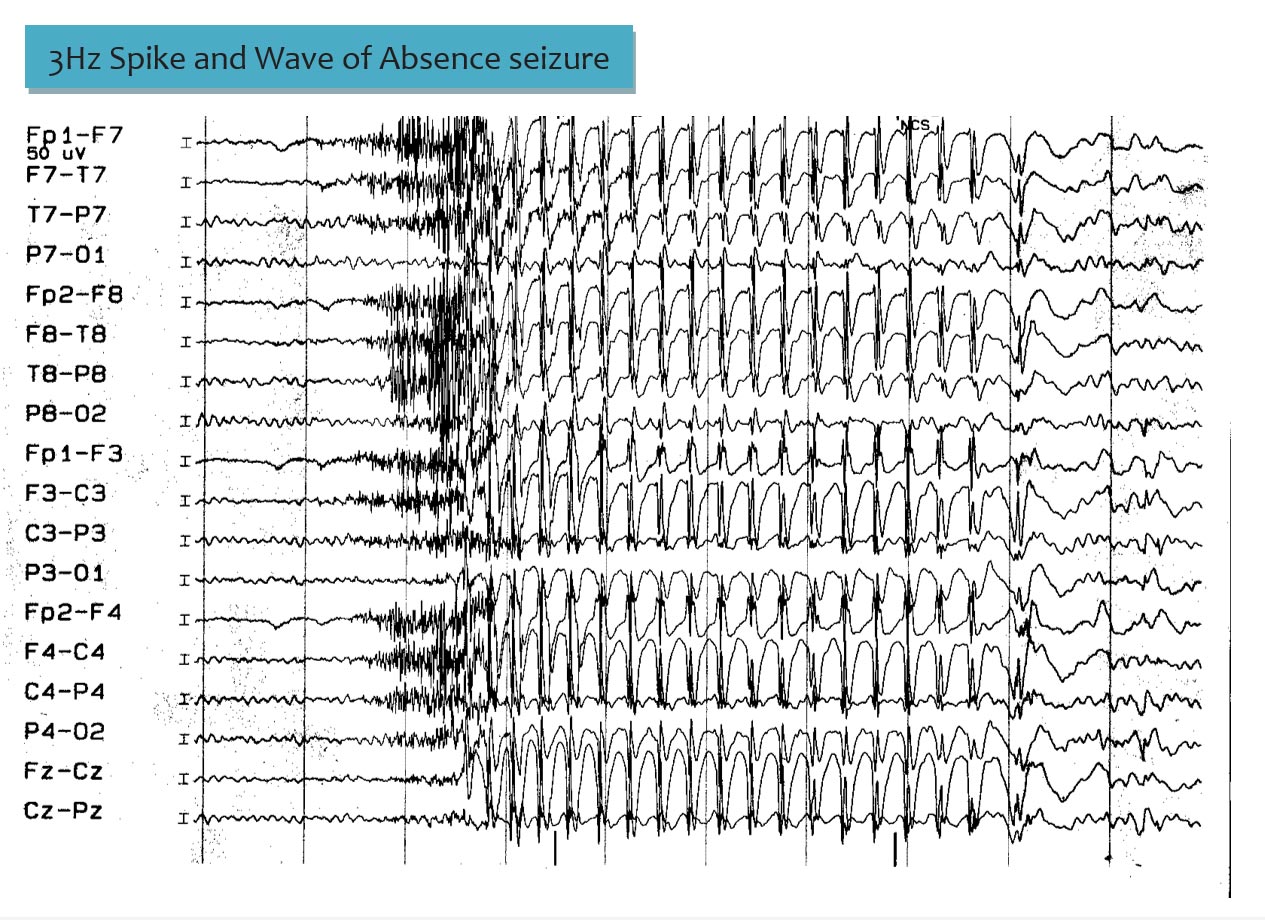
There is an abrupt sudden loss of consciousness (the absence) and cessation of all motor activity. There is no fall. The patient is not in contact with the environment, often appears glazed, vacant, staring or dreaming. The attack ends as abruptly as it started, and previous activity is resumed as if nothing had happened and there is no post seizure confusion. The patient is often unaware that an attack has occurred. The EEG during a typical absence is diagnostic, shown high voltage, regular, symmetric and synchronous 3 Hz spike-wave paroxysms.
Generalised tonic clonic seizure
This is the type of seizure most people are familiar with. This is the convulsion or fit in layman term. There is abrupt loss of consciousness, sometimes with the epileptic cry (a loud sound), tonic stiffening (and the patient falls if standing) initially in flexion of the limbs but then in axial extension, with the eyes rolled up, the jaw shut (leading to tongue bite), the limbs stiff, adducted and extended, and the fists clenched. Respiration ceases and there is cyanosis. The eyes remain open and the pupils dilated and unreactive. There are frequently heart rate changes, which are sometimes marked and can take the form of tachycardia or bradycardia and even asystole. This tonic stage lasts on average 10–30 seconds and is followed by the clonic phase, during which convulsive movements, usually of all four limbs, jaw, and facial muscles occur. Breathing is laborious and arrest of respiration can occur, saliva (sometimes bloodstained owing to tongue biting) may froth from the mouth. The convulsive movements decrease in frequency (eventually to about four clonic jerks per second), and increase in amplitude as the attack progresses. The attack is usually followed by a period of flaccidity of the muscles and consciousness is slowly regained.
Myoclonic seizure
There is brief contraction of a muscle, muscle group or several muscle groups brought about by a cortical discharge. It can be single or repetitive, varying in severity from an almost imperceptible twitch to a severe jerking, resulting, for instance, in a sudden fall or the propulsion of handheld objects. Recovery is immediate, and the patient often maintains that consciousness was not lost.
Causes of epilepsy
Epilepsy is often a multifactorial condition, genetic and environmental factors often play a part in its clinical manifestations. Genetic, congenital and perinatal conditions are the most common causes of early childhood onset epilepsy, whereas in adult life, head injury, vascular disease, tumors are common causes. In India endemic infections such as cysticercosis, tuberculosis, meningitis and encephalitis are common causes. Cerebral palsy a non-specifi c term that covers several prenatal and perinatal pathologies is strongly associated with epilepsy. AV malformations, cavernomas, degenerative disorders like Alzheimer dementia can cause seizures and epilepsy. Head trauma is an important cause of epilepsy (post traumatic epilepsy). Neuro-cysticercosis is the most common parasitic disease of the CNS. Epilepsy is the most common clinical manifestation and usual presenting symptom and neuro-cysticercosis a major cause of epilepsy in India.
Differential diagnosis of epilepsy
Differential diagnoses of transient neurological dysfunction are broad and Epileptic seizures feature in many differential diagnoses of transient neurological dysfunction. The most common error is to diagnose a syncopal episode as an epileptic seizure. Undue reliance placed on investigations, particularly the EEG and MRI lead to errors. Non specific EEG abnormalities, normal variants are erroneously labeled as epileptiform activity leading to misdiagnosis of epilepsy. Questionable CT and MRI abnormalities (like small calcific lesions, perivascular spaces) are wrongly labeled as abnormal and the patient is advised unnecessary therapy with antiepileptic medications. The diagnosis of epilepsy is made primarily on the history, and the role of the EEG is to assist in the subsequent classification of the type of epileptic seizures and the epilepsy syndrome.
When taking the history it is a good practice to first allow the individual and witnesses to give their own freehand eyewitness account of the points without interrupting and to then go over again on the salient points in a systematic manner.
In those who have had repeated episodes, a videotape recording with a mobile phone camera of an episode is frequently invaluable, conveying more information.
Some conditions that could be mistaken for epilepsy are listed below
Neurally mediated syncope
Situational syncope
Micturition syncope
Tussive syncope
Deglutination syncope
Defecation syncope
Glossopharyngeal neuralgia
Carotid sinus hypersensitivity
Orthostatic syncope
Cardiac syncope
Arrhythmia
Valvular heart disease
Cardiomyopathy
Atrial myxoma
Cardiac tamponade
Pulmonary embolus
Cerebrovascular disease (TIA, Infarction, hemorrhage)
Vertebrobasilar insufficiency
Subclavian steal
Vertebrobasilar migraine
Brainstemcompression
Arnold-Chiari malformation
Hydrocephalic attacks
Epileptic seizure
Psychiatric disorders
Panic attacks
Somatization disorder
Psychogenic unresponsiveness
Malingering
Migraine
Basilar migraine
Migraine with epilepsy
Metabolic conditions
Hypoglycemia
Hyperammonemia
Hyponatremia
Hypocalcemia
Microsleeps
Nonepileptic attacks/Psychogenic pseudoepileptic epileptic attack/ Non-epileptic attack disorder
With excessive motor phenomenon
With lying motionless
Evaluation after the First Seizure
Epilepsy is a group of conditions and not a single homogeneous disorder and seizures may be symptoms of both diverse brain disorders and an otherwise normal nervous system, it is not possible to develop inflexible guidelines for what constitutes a standard set of diagnostic tests.
Furthermore, it is not always clear from the history that the patient has even had a seizure or has epilepsy.
Thus, the role of the physician is threefold:
(a) To determine whether epilepsy or seizures exist and not some alternative diagnosis
(b) To define, if possible, an underlying cause
(c) To decide whether to treat and optimize treatment
Epilepsy is primarily a historical diagnosis, and the initial assessment and approach to management are based, in large part, on the clinical history, especially on an accurate description of the event in question. Information should be obtained from the patient when possible, as well as from other individuals (especially family members) who have observed typical attacks.
EEG (Electroencephalogram)
See earlier discussion in diagnosis
Neuroimaging (CT, MRI, PET, SPECT)
The modern era of structural brain imaging - first with computed tomography (CT), then with magnetic resonance (MR) - has revolutionized our ability to identify epileptogenic brain lesions. With high-resolution MR scans, a wide variety of pathologic lesions can now be diagnosed routinely and noninvasively. These include mesial temporal sclerosis, well-differentiated gliomas, gangliogliomas, cavernous malformations and neuronal migration defects. Fewer seizure disorders are now justifiably classified as "idiopathic" or even "cryptogenic." Functional brain imaging, such as positron emission tomography (PET) single photon emission computed tomography (SPECT)), and magnetic resonance spectroscopy, is providing additional and often critical information about the extent of metabolic changes and alterations in regional cerebral blood flow associated with seizures. It is important to note that merely a presence of lesion on MRI does not mean the patient has seizures or epilepsy.
Treatment
Single seizure or first seizure - To treat or not to treat.
Whether therapy with antiepileptic drugs (AEDs) should be initiated after a first seizure is controversial. Within 5 years after a single, unprovoked seizure, 16-62% of patients have another seizure.
Recurrence is more likely if there has been an earlier neurologic injury sufficient to cause seizures; a structural abnormality on neuroimaging; an abnormal, particularly epileptiform, EEG; or a family history of epilepsy.
Most studies also suggest that partial (including secondarily generalized) seizures are more likely to recur than primarily generalized tonic-clonic seizures. Treatment can reduce (perhaps by 50%) but not eliminate the risk of a second seizure.
The treatment decision must be made individually for each patient, considering the potential physical, psychological, and occupational consequences of further seizures and of AED therapy. Many patients may want to take medications after a single seizure, since medications definitely reduce the risk of recurrence.
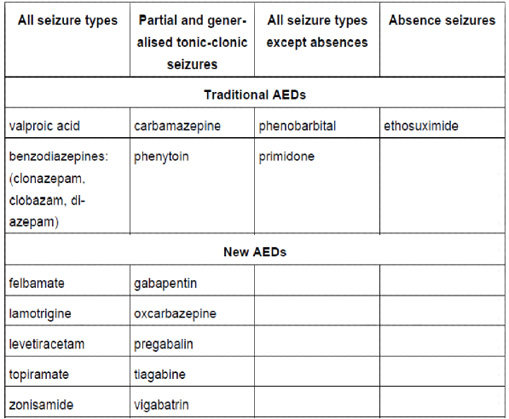
Choice of medications after decision to treat has been made
There are several drugs available for epilepsy. The comparison studies have shown that the efficacy of these drugs is similar. The newer drugs have a better side effect profile and adverse effect profile. Generally they do not cause cognitive side effects and other serious side effects.
The following table lists the commonly used AEDs and the choice of AEDs in various seizure types.
Patient's Education
- Epilepsy
- Parkinson Disease
- Migraine
- Stroke
- Bell facial palsy
- Tension type headache
- Alzheimer dementia
- Vertigo
- Neurocysticercosis
- Cerebral venous sinus thrombosis
- Motor neuron disease
- Myasthenia gravis
- Carpal tunnel syndrome
- Wilson disease
- Meningitis
- Febrile Seizures
- Medication overuse headache
- Back pain
- Demyelination and Multiple Sclerosis
- Facial pain
- Neck Pain
- Trigeminal Neuralgia