Demyelinating diseases
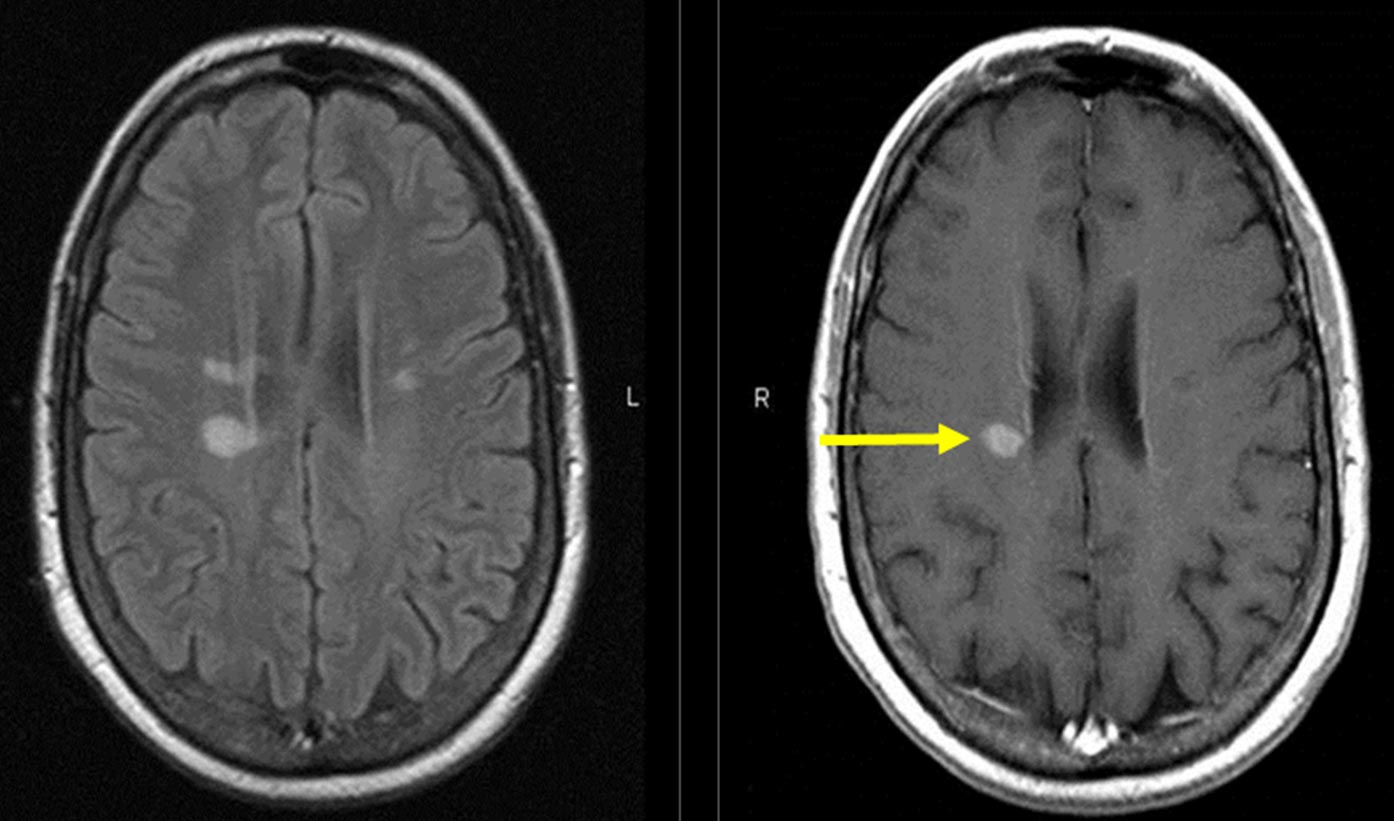
Once thought to be rare these diseases are seen quite frequently in neurology practice. The increase in awareness and availability of MRI (magnetic resonance imaging) has made diagnosis of these disorders easy.
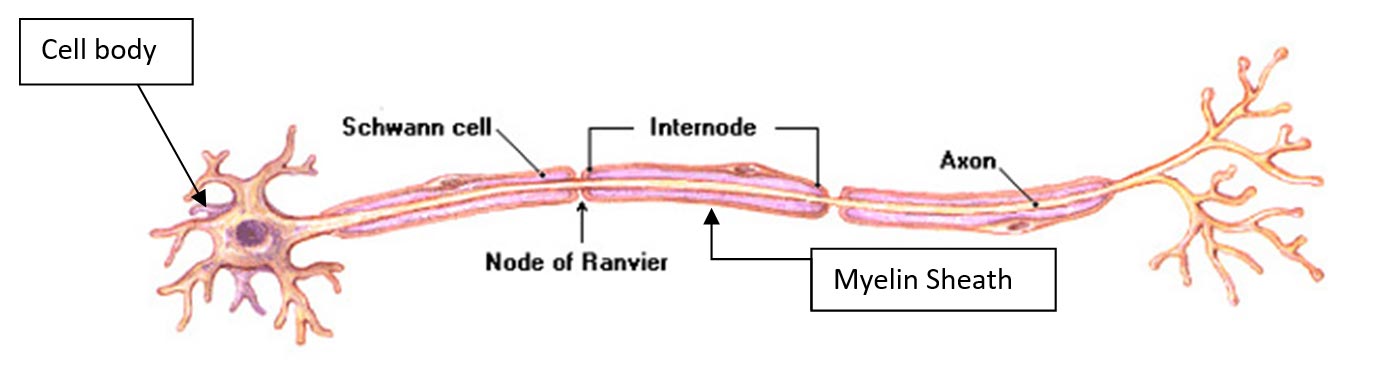
In this group of diseases, the myelin sheath around the nerve fibers is selectively affected (Though there is strong evidence that there is axonal loss as well).
Multiple Sclerosis, neuromyelitis optica spectrum disorders (NMOSD) (Aquaporin-4 antibody disease), acute disseminated encephalomyelitis, MOG antibody disease (MOGAD) and acute hemorrhagic encephalomyelitis are the inflammatory demyelinating diseases.
Multiple Sclerosis
Multiple sclerosis typically presents at 20–40 years of age. Females are more susceptible than males. Male to female ratio is approximately 2: 1. MS is more common in temperate regions, such as northern Europe, North America and southern Australasia, but much rarer in the tropical countries like India.
People who migrate from one geographical area to another before adolescence are essentially subject to the same level of risk of the area to which they migrate. Multiple sclerosis is the most common cause of neurological disability in young adults.
Etiology
A complex interplay between environmental factors and individual genetic susceptibility leads to tissue injury by autoimmune mechanisms. History or serological evidence of Epstein Barr virus infection increases the risk for getting Multiple Sclerosis Experimental and epidemiological data suggest that high levels of vitamin D decrease the risk of multiple sclerosis. Taking vitamin D supplementation has been associated with a reduction in the risk of developing multiple sclerosis.
Pathology
Demyelinating plaque is the characteristic pathological feature of MS. These lesions occur particularly in the optic nerves, peri-ventricular white matter and corpus callosum, brainstem and cerebellar white matter, and cervical cord. These are responsible for failure of the nerve impulse to travel and lead to the various symptoms of MS.
Clinical features
Blurring of vision: Acute onset of diminished vision due to optic neuritis is a frequent presenting symptom of MS. In some patients this may remain as the only episode when it is called true clinically isolated syndrome.
Weakness: Hemiparesis due to demyelination in the spinal cord of white matter of the brain.
Paraparesis: Due to transverse myelitis is associated with urinary retention followed by incontinence and loss of all sensation below a level on the trunk.
Sensory symptoms: Hemiparesthesias (abnormal sensation on one half of the body), heat intolerance, trigeminal neuralgia, posterior column loss are common symptoms in patients of MS.
Diplopia: Double vision due to internuclear ophthalmoplegia, lateral rectus palsy in young women can be a presenting symptom of MS.
Imbalance: Cerebellar ataxia is due to demyelination of the cerebellar tracts. Associate signs of cerebellar dysfunction like nystagmus, scanning speech are present.
MS is a relapsing remitting disease in most of the patients. Episodes of neurological deficits occur abruptly over few days and are followed by partial or complete recovery. Over a period of years residual deficits remain leading to disability.
Clinical course:
Relapsing remitting (RRMS)
Primary progressive (PPMS)
Secondary progressive (SPMS)
Progressive relapsing (PRMS)
Diagnosis
Two neurological events disseminated in time and space for which no alternative explanation exists is required for diagnosis of MS. MS can be diagnosed at the first episode of demyelination. This is done by applying the 2017 revised McDonald Criteria. A thorough history, neurological examination with MRI, visual evoked potentials, CSF study for oligoclonal bands is required for diagnosis of MS.
The differential diagnosis of MS is huge and appropriate tests have to be done for excluding these disorders.
Treatment
The diagnosis of MS affects all aspects of the patient’s life like education, finance, social, and marital. Hence management strategies are required to provide education and support in addition to the pharmacotherapy and rehabilitation therapy. Management includes therapy of acute relapses, disease modifying therapy and treatment of symptoms.
Acute relapse: Injections of methylprednisolone for 3 to 5 days. In unresponsive cases plasma exchange can be tried.
Disease modifying therapy: Interferon-b1a (Avonex) Interferon-b1a (Rebif), Interferon-b1b (Betaferon) glatiramer acetate, Dimethyl fumarate, Teriflunomide, Fingolimod, Mitoxantrone, Natalizumab (Tysabri, Biogen), Rituximab, Ofatumumab (Bonspri, Novartis), Alemtuzumab (Lemtrada, Sanofi), Ocrelizumab (Ocrevus, Roche) reduce the frequency of episodes and reduce the lesion burden on MRI. These therapies have to be taken on a long-term basis under supervision of a neurologist experienced in treating MS patients.
Symptomatic therapy: For fatigue, bladder and bowel disturbance, spasticity, sexual dysfunction, pain, paroxysmal symptoms effective pharmacotherapy is available.
Patient's Education
- Epilepsy
- Parkinson Disease
- Migraine
- Stroke
- Bell facial palsy
- Tension type headache
- Alzheimer dementia
- Vertigo
- Neurocysticercosis
- Cerebral venous sinus thrombosis
- Motor neuron disease
- Myasthenia gravis
- Carpal tunnel syndrome
- Wilson disease
- Meningitis
- Febrile Seizures
- Medication overuse headache
- Back pain
- Demyelination and Multiple Sclerosis
- Facial pain
- Neck Pain
- Trigeminal Neuralgia