Cerebral venous sinus thrombosis (CVT) is more common than previously thought. This is because of increasing awareness about the disorder and easier recognition of this condition on brain imaging (CT, MRI, MRV). CVT is occlusion of the cerebral veins and/or venous sinuses due to thrombosis (clotting).
CVT is more common in women especially during pregnancy.
Risk factors for CVT
- Infection- ear infection (otitis media, mastoiditis, sinusitis), meningitis, sepsis
- Trauma - head injury, jugular vein canulation
- Pregnancy and peurperum
- Drugs - oral contraceptive pills, hormone replacement therapy, erythropoietin, tamoxifen
- Nephrotic syndrome, Systemic lupus erythematosis, Behcet disease
- Hyperhomocystenemia, vitamin B12 deficiency
- Procoagulant states - polycythemia, prothrombin gene mutation, antiphospholipid antibody syndrome, sickle cell disease, protein S and C deficiencies, antithrombin III deficiency
- Dehydration due to any cause
- Diabetes, diabetic ketoacidosis
Clinical features
The presentation is highly variable and can mimic several diseases. Hence a high degree of suspicion is a must. The presentations can be of chronic headache for months, or catastrophic with acute onset headache with vomiting, seizures, focal deficits and unconsciousness.
Acute presentation
- Thunderclap headache - pounding, exploding, stabbing severe intensity headache of sudden onset.
- Focal neurologic deficits - hemiparesis, weakness in both lower limbs, aphasia, ataxia, visual disturbance
- Drowsiness progressing to coma over few hours or days to week.
- Cavernous sinus thrombosis with proptosis, chemosis with septicemia.
Subacute presentation
Chronic headache for months. Migraine like headaches Cognitive decline over months with encephalopathy. Tinnitus, double vision, visual obscuration, facial weakness.
Chronic presentation
Could be like a pseudotumor syndrome or headaches of mild severity for months like chronic daily headache. Papilledema is usually present. Cortical vein thrombosis could present with seizures.
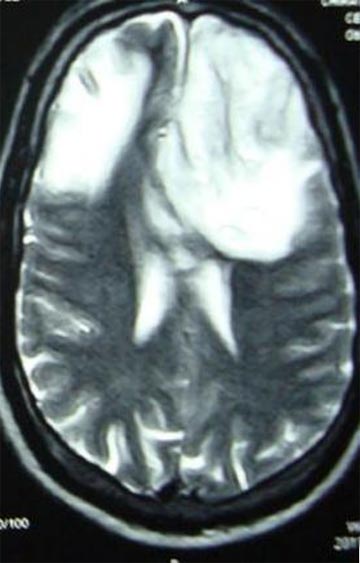
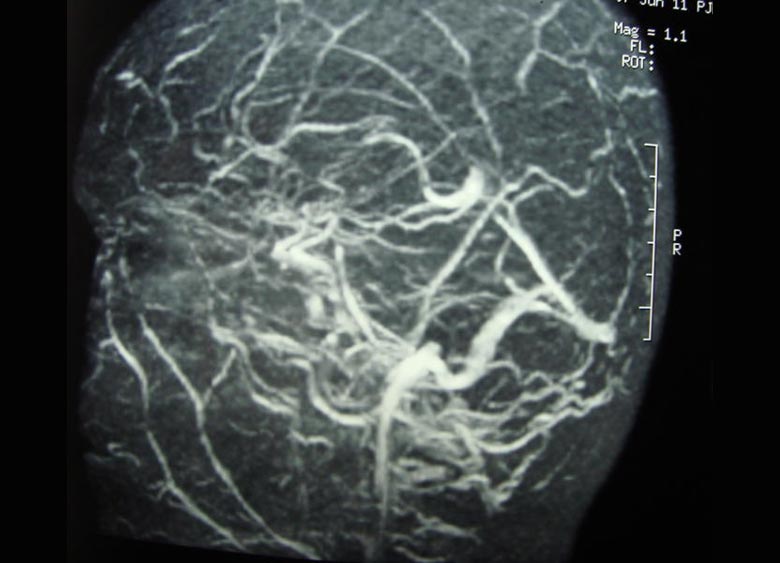
Diagnosis
High degree of suspicion in patients with headaches of any nature. Any patient with a catastrophic neurologic syndrome could have CVT. Papilledema is a constant finding. CT scan, MRI and MRV usually will confirm diagnosis. Digital subtraction angiography with venous phase is gold standard.
Treatment
This depends on the type presentation. For acute CVT anticoagulation to arrest the thrombosis is the key. If there is clinical deterioration despite adequate anticoagulation IV or intrasinus thrombolysis or mechanical thrombectomy may be considered.
Supportive / Symptomatic treatment with IV fluids, anticonvulsants, and lowering of raised intracranial pressure, antibiotics for infective etiology. The duration of anticoagulation depends on the risk factor for thrombosis.
Prognosis
Good recovery is seen in 60% patients receiving anticoagulation. Fatality up to 15 % is seen in patients with catastrophic presentation.
Patient's Education
- Epilepsy
- Parkinson Disease
- Migraine
- Stroke
- Bell facial palsy
- Tension type headache
- Alzheimer dementia
- Vertigo
- Neurocysticercosis
- Cerebral venous sinus thrombosis
- Motor neuron disease
- Myasthenia gravis
- Carpal tunnel syndrome
- Wilson disease
- Meningitis
- Febrile Seizures
- Medication overuse headache
- Back pain
- Demyelination and Multiple Sclerosis
- Facial pain
- Neck Pain
- Trigeminal Neuralgia