The term vertigo means different to different people. “Vertigo” is often used in a confusing way by people. The term vertigo is misused by patients and laymen to convey heaviness in the head, a sense of imbalance while walking without actual falls or it may mean light headedness. Some people use the word for fainting, unconsciousness or even a true convulsive seizure. The misquote of vertigo is further propagated by the movie Vertigo which is not in fact about true vertigo, it is about agoraphobia. The true medical meaning of vertigo is a false sense (hallucination) of self-motion when there is no real motion or sensation of distorted self-motion during an otherwise normal head movement. Earlier rotation of self or the surrounding was termed vertigo in the true sense. Dizziness is a sensation of disturbed or altered spatial orientation without the feeling of false motion.
Vertigo by itself is not a disease. It is a symptom of an underlying disease. It is a symptom like fever which has several different causes. Commonly diseases of the inner ear cause vertigo (peripheral). These are usually not life threatening but are disabling. As opposed to these, diseases of the nervous system causing vertigo could be serious (central). These could be stroke, tumor, demyelination like multiple sclerosis. The common peripheral diseases are benign paroxysmal positional vertigo, vestibulitis, and post traumatic vertigo. The nature of the symptoms accompanying vertigo and the duration of symptoms helps to know the correct cause of vertigo. Ear diseases causing vertigo are almost always not accompanied by other neurologic symptoms. Nervous system related causes which are more serious are almost always accompanied with other neurological symptoms and signs.
Benign paroxysmal positional vertigo (BPPV)
BPPV is a common cause of vertigo. About 20% of all vertigo is due to BPPV. Benign paroxysmal positional vertigo (BPPV) is a condition characterized by episodes of sudden and severe vertigo when the head is moved around. The vertigo typically lasts for second and usually less than a minute. The vertigo is precipitated by a particular position of the head (semicircular canals). Common triggers include rolling over in bed, turning in the bed, getting out of bed, and lifting the head to look up. An affected person may have attacks of vertigo for a few weeks, then a period of time with no symptoms at all. Usually BPPV affects only one ear commonly the right ear. It is thought that BPPV is caused by particles (calcium crystals called as debris) within the balance organ of the inner ear. Other names for BPPV include benign postural vertigo, positional vertigo and top shelf vertigo (because you get vertigo on looking up).
Symptoms
The symptoms of BPPV include dizziness or vertigo, lightheadedness, imbalance, and nausea.
The symptoms of BPPV are:
- Sudden episodes of violent vertigo
- Nausea
- The vertigo may last half a minute or so
- The eyes may drift and flick uncontrollably (nystagmus)
- Movements of the head trigger the attacks
All these symptoms may not be seen in a particular patient and variation in presentation is common.
Etiology
Inside the inner ear is a series of canals filled with fluid. These canals are at different angles to each other. These canals detect the exact position of head and movement of the head. When the head is moved, the rolling of the fluid inside these canals tells the brain exactly how far, how fast and in what direction the head is moving. BPPV is thought to be caused by small calcium carbonate crystals/debris (otoconia) within the canals. Usually, these crystals are held in special reservoirs within other structures of the inner ear (saccule and utricle). It is thought that injury or degeneration of the utricle may allow the 'ear rocks' (the crystals) to escape into the balance organ and interfere with the fluid flow.
Factors that may allow calcium carbonate crystals to migrate into the balance organ include:
- Head injury
- Ear injury
- Ear infection, such as otitis media, viral infections
- Ear surgery
- Degeneration of the inner ear structures
- Vestibular neuritis (viral infection of the inner ear)
- Meniere's disease (disorder of the inner ear)
- Some types of minor strokes
- In around half of BPPV cases, the cause can't be found (idiopathic BPPV).
Diagnosis
Since vertigo can be a symptom of a serious brain disorder a careful history and examination is required for diagnosis of BPPV.- Medical history - illnesses such as cardiac arrhythmia, low blood pressure and multiple sclerosis can include symptoms of vertigo.
- Physical examination - The patient lies on the examination bed while the doctor deliberately moves their head into positions that are known to trigger BPPV within a few seconds. The doctor will also check for positional nystagmus.
- Electronystamography (ENG) - a special eye test that checks for the presence of nystagmus.
- Ear tests - such as hearing tests.
- Imaging - magnetic resonance imaging, to check for the presence of other Neurological disorder (Brainstem, cerebellum) which can cause vertigo.
It should be noted that BPPV is a diagnosis of exclusion since nervous system disorders could cause symptoms similar to BPPV. Hence these disorders should be excluded by proper evaluation by a neurologist and MRI scan of the brain when appropriate.
Treatment
Generally, BPPV resolves by itself within six months or so. The patient could get recurrent attacks and vertigo can recur for a long time in some patients. Treatment options in the meantime could include medications to help control vertigo. These are betahistine and vestibular sedatives in case of incapacitating vertigo. Special maneuvers (canalith repositioning) designed to dislodge otoconia is the specific treatment of BPPV. These maneuvers have an 80 per cent success rate:- The Semont maneuver - In this the patient lies down, then is quickly rolled from one side to the other.
- The Epley maneuver - This is also known as the typical canalith repositioning procedure. The patient's head is moved into four different postures. The head is held in each posture for about half a minute.
- The Epley maneuver – This is also known as the typical canalith repositioning procedure. The patient’s head is moved into four different postures. The head is held in each posture for about half a minute.
These maneuvers can be done in the office, with instructions to be followed at home.
- After-treatment care - It is important to sit still for at least 10 minutes after the Semont or Epley manoeuvre to allow the otoconia to settle. For the next 48 hours, keep the head still and upright and sleep in a semi-sitting position (at an angle of 45⁰). During the day, try to keep your head vertical. For the next five days, strictly avoid any postures that have triggered BPPV in the past. After one week, deliberately try to induce BPPV to see if your symptoms have improved. Report to your doctor.
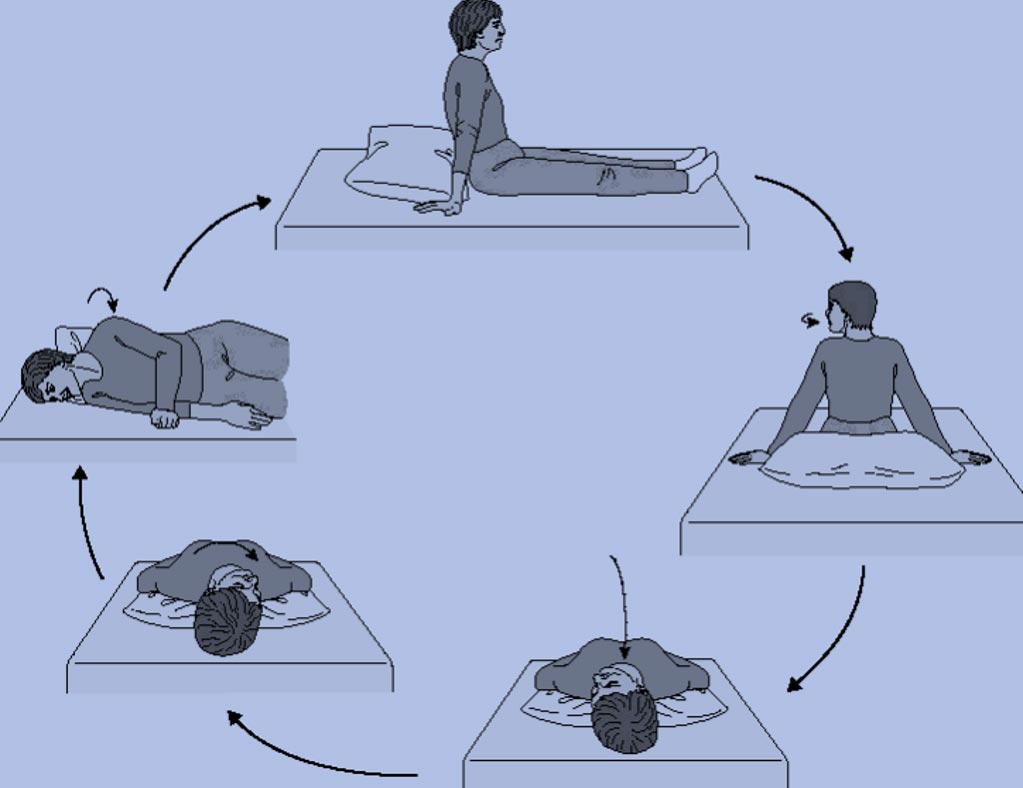
- Brandt-Darroff exercises - If the above manoeuvres don’t work, the next stage of treatment is Brandt-Darroff exercises. This is a more complex series of postures that have to be performed three times every day for two weeks.

- Start sitting upright (position 1). Then move into the side-lying position (position 2), with the head angled upward about halfway. Stay in the side-lying position for 30 seconds, or until the dizziness subsides if this is longer, then go back to the sitting position (position 3). Stay there for 30 seconds, and then go to the opposite side (position 4) and follow the same routine. This one cycle will take 2 minutes.
- These exercises should be performed for two weeks, three times per day, or for three weeks, twice per day. In most persons, complete relief from symptoms is obtained after 30 sets, or about 10 days. In approximately 30 percent of patients, BPPV will recur within one year. Unfortunately, daily exercises are not effective in preventing recurrence.
- When performing the Brandt-Daroff maneuver, caution is advised should neurological symptoms (i.e. difficulty speaking, weakness, numbness, headache, neck pain, visual changes other than vertigo) occur. Occasionally such symptoms are caused by compression of the vertebral arteries In this situation it is advisable not to proceed with the exercises and consult your neurologist.
Lifestyle changes
Certain lifestyle changes could help to manage BPPV and reduce the frequency of attacks.
- Avoid travel during the acute episodes of vertigo, especially if these are frequent.
- Sleep with your head raised higher than usual - for example, use two pillows instead of one.
- In bed, try to avoid lying on the affected side.
- Remember that lying on your back may bring on symptoms too.
- When rising in the morning, move slowly. Rest for a few minutes at each posture.
- Whenever possible, avoid moving your head quickly.
- You may have to avoid sporting activities that rely on quick changes of movement and posture (such as football or tennis).
- Remember that any activity that requires you to tip your head back could bring on vertigo. This could include activities such as getting your hair washed at the hairdressers or having a dental check-up.
Surgery may be needed in severe cases
If non-surgical treatments fail, and the symptoms continue for more than 12 months, an operation may be needed. Generally, the vestibular nerve is cut. The risks of this type of operation include hearing loss.
Summary
- Benign paroxysmal positional vertigo (BPPV) is a condition characterized by short duration (less than 2 minutes) episodes of sudden and severe vertigo when the head is moved around.
- Common triggers include turning in bed, getting out of bed, and lifting the head to look up.
- It is thought that BPPV is caused by particles (debris) within the balance organ (semicircular canal) of the inner ear.
- Canalith repositioning and vertigo exercises are effective treatment for BPPV.
Patient's Education
- Epilepsy
- Parkinson Disease
- Migraine
- Stroke
- Bell facial palsy
- Tension type headache
- Alzheimer dementia
- Vertigo
- Neurocysticercosis
- Cerebral venous sinus thrombosis
- Motor neuron disease
- Myasthenia gravis
- Carpal tunnel syndrome
- Wilson disease
- Meningitis
- Febrile Seizures
- Medication overuse headache
- Back pain
- Demyelination and Multiple Sclerosis
- Facial pain
- Neck Pain
- Trigeminal Neuralgia